People who are less likely to put on excess fat around their hips due to their genes are at higher risk of type 2 diabetes and heart attacks, according to a new study led by scientists from the MRC Epidemiology Unit at the University of Cambridge.
While it has long been recognised that an “apple-shaped” body is associated with an increased risk of diabetes and heart disease, the new research sheds light on the specific genetics linked to this body shape and the potential mechanisms behind the increased risk. The researchers suggest that their findings, published in JAMA: the Journal of the American Medical Association, may help to better identify individuals at risk of developing these conditions and inform their subsequent treatment.
The researchers studied the genetic profiles of over 600,000 participants from several large UK and international studies – including the UK Biobank, Fenland, EPIC-Norfolk, and EPIC-Interact – and identified over 200 genetic variants that predispose people to a higher waist-to-hip ratio, a measure of the “apple shaped” body. Using this data, the researchers identified two specific groups of genetic variants that increased waist-to-hip ratio – one exclusively via lower hip fat and the other exclusively via higher waist (abdominal) fat.
The study’s senior author, Dr Claudia Langenberg, Programme Leader at the MRC Epidemiology Unit, said:
We found that both of the genetic variants we identified were associated with higher risk of type 2 diabetes and heart attacks. The concept of an ‘apple shaped’ figure has been understood for some time but our research considers how this body shape alters fat distribution in the body. Genetics which specifically change fat distribution by lowering fat storage around the hips increase risk of disease independent of, and in addition to, mechanisms that affect abdominal fat storage.”
Lead author, Dr Luca A. Lotta, Senior Clinical investigator at the MRC Epidemiology Unit, said:
It may seem counterintuitive to think that some people with less fat around their hips are at higher risk of diabetes or heart disease. We believe that this is due to a genetically-determined inability to store excess calories safely in the hip region as opposed to elsewhere. This means that individuals with this genetic make-up preferentially store their excess fat in the liver, muscles or pancreas, or in their blood in the form of circulating fats and sugar, any of which can lead to a higher disease risk.”
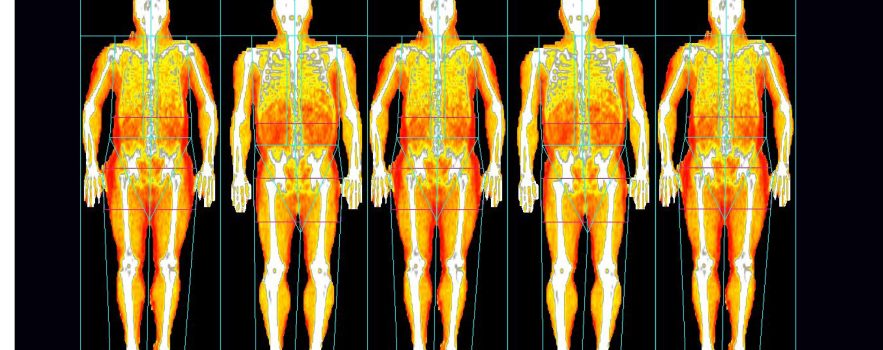
To validate their findings, the authors conducted detailed assessments of fat distribution in different regions of the body of 18,000 people using DEXA, a low-intensity X-ray scan that can distinguish body fat, bone composition, muscle and lean mass across the whole body.
The researchers also suggest that there is a greater proportion of people in the general population with subtle forms of familial partial lipodystrophy, a rare genetic disorder characterised by the inability to develop fat in the arms, legs and buttocks. Those with this condition often go on to develop diabetes and its cardiovascular complications.
The team behind this research hope that their findings will help to better understand the ways in which fat storage in different body compartments affects metabolic health and leads to disease. They suggest their work could refine the way we detect and treat people at risk.
Dr Langenberg said:
Not all apple shapes are the same. Guidelines that focus solely on measuring waist circumference to assess risk overlook people whose body shape is not adequately captured by this metric, but who are still likely to develop cardiovascular and metabolic diseases. Carrying excess weight around the hips is a metabolically safer way of storing fat, but those who aren’t genetically predisposed to doing so would benefit greatly from lifestyle interventions, such as restricting their calorie intake or increasing their physical activity.”
Existing diabetes drugs called glitazones prevent or improve the disease in part by enhancing the ability to expand hip body fat. However, their use in clinical practice is limited by some of their side-effects. The researchers hope that their genetic findings might lead to the development of new agents targeting body fat deposition in the future.
Dr Lotta said:
We are trying to understand whether some of the genes identified by our study may be suitable targets for future drug development, but this process may take several years.”

 MRC Epidemiology Unit
MRC Epidemiology Unit