By Adina L. Feldman, MRC Epidemiology Unit, University of Cambridge
Type 2 diabetes is a global health issue affecting 414 million adults world-wide.1 Although the number of people being newly diagnosed with diabetes (the incidence) appears to be stabilising and perhaps even decreasing, the total number of people living with the disease (the prevalence) is increasing.2,3 The health consequences of diabetes place a strain on the quality of life for patients as well as on healthcare systems, so improving primary prevention (preventing the disease from developing in the first place) should be a priority for public health. However, which interventions strategies are most effective in achieving this remains an open question.
Prevention Strategies for Diabetes
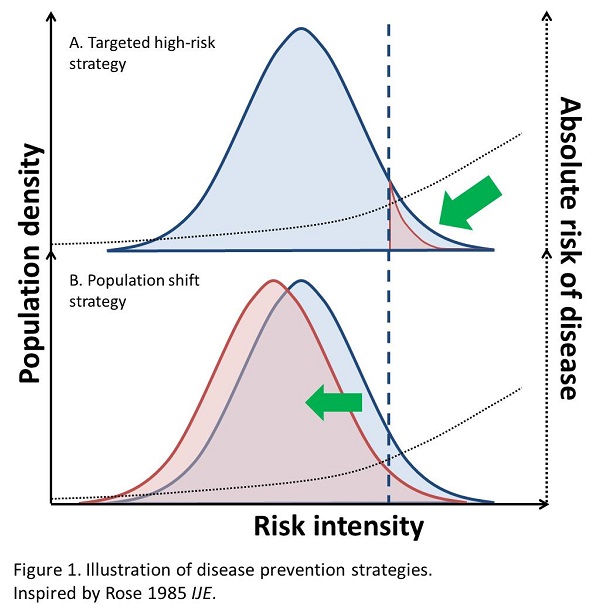
In 1985 Geoffrey Rose published Sick individuals and sick population4 in the International Journal of Epidemiology introducing the concept of population shift strategy as a complement to a targeted high-risk strategy for prevention of disease. While the high-risk strategy aims to reduce occurrence of disease in people at the highest risk through targeted interventions, the population shift strategy aims to move the population distribution towards lower risk, reducing the number of people at high risk but also potentially reducing the occurrence of disease in the population as a whole. These different strategies are illustrated in Figure 1.
Prevention of type 2 diabetes using the high-risk strategy has been explored through many randomised controlled trials in people with hyperglycaemia and other risk factors, showing that intensive lifestyle interventions and weight loss are highly effective and can approximately halve diabetes risk5 in this group. However, since the threshold for who is considered to be at high risk of type 2 diabetes is somewhat arbitrary and that the proportion of people identified as being at high risk only constitutes a small part of the overall population at risk, there is rationale to explore prevention strategies focused on population shift as well.
Measuring Differences Between Individuals vs. Change Within Individuals
Most epidemiological evidence of risk factors for diabetes and other chronic diseases comes from observational prospective cohort studies where an exposure to a risk factor is typically measured at one time-point in a general disease-free population, which is then followed up for occurrence of the outcome over a defined period. Such studies have yielded ample evidence for associations between several lifestyle behaviours and other risk factors and type 2 diabetes incidence, including protective effects of dietary fibre intake,6 moderate alcohol drinking,7 physical activity,8 body mass index (BMI) less than 25kg/m2 9 and non-smoking10. However, since these studies examine differences between individuals at only one point in time their results cannot be conclusively causally interpreted as support for a population shift strategy since we cannot rule out that unmeasured factors which influence both lifestyle behaviour and type 2 diabetes have distorted the results, so called residual confounding.
Ideally we would like to conduct randomised trials of interventions in the general population as well as in high-risk groups to understand if improving lifestyle behaviour, for example low physical activity or poor diet, could reduce diabetes occurrence in the general population which is not considered at high risk of disease. Unfortunately, such randomised trials are rare due to being very logistically challenging, costly, difficult to conduct, and in some cases unethical.
So how can we try to understand the potential of population shift of risk in the general population in the absence of randomised studies? One way is to use observation data to study people who change exposure status over time without a controlled intervention. To be able to do this you need repeated measures of both exposures and outcomes over time for large populations, and there are not many existing or on-going cohorts that have this kind of data available for analysis, and fewer that have used their data in this way. It is more common when having repeated measures of an exposure to analyse it as a time-varying exposure, meaning that exposure status is updated for individual observations at the time of the second (and possible third, fourth, etc.) measurement. This is an effective way to use the data, but the estimated effect is in relation to the absolute level of the exposure, and not in relation to change in exposure status.
Evidence from Studies on Change Within Individuals
Recently two studies from the VIPCAM collaboration between the University of Cambridge in the UK and Umeå University in Sweden have shed some light on the potential of population shift strategies for prevention of diabetes. Data from the Västerbotten Intervention Programme (VIP),11 a public health programme in northern Sweden that includes health examination every 10 years on a large population-based sample, were used to study change within individuals in exposure to risk factors and incidence of type 2 diabetes.
The VIP data were also used to estimate the public health potential of a population shift in risk to reduce the occurrence of diabetes by estimating population attributable fractions (PAF) which calculate the proportion of disease cases attributable to a particular exposure.
Results for type 2 diabetes show that:
- Increase in a healthy lifestyle behaviour score that includes measures for diet, alcohol consumption, physical activity and smoking was associated with an 8% reduction in risk for every point increase at the 5-point scale.12
- Increase in dietary fibre intake by ≥3 g/1,000 kcal/day was associated with a 20% reduction in risk, and this corresponded to a PAF of 16%.12
- Compared to people who maintained their weight, a decrease in weight of 1-2 kg/m2 (1-2 BMI units) was associated with a 28% reduction in risk, and this corresponded to a PAF of 42%.13
- Compared to people who gained >1 kg/m2, maintenance of weight (±1 kg/m2) was associated with a 34% reduction in risk, and this corresponded to a PAF of 22%.13
In the US cohorts the Nurses Health Study I & II and the Health Professionals Follow-up Study data have been collected on lifestyle behaviour and diabetes every 4 years over a long follow-up period and these data have similarly been used to study changes in exposure and diabetes incidence.
Results for type 2 diabetes have shown that (compared to those who do not change exposure status over time);
- Decrease in weight of 2.5-5 kg was associated with a 31% reduction in risk.14
- Increase in the Alternate Healthy Eating Index (AHEI) score by >10% was associated with a 16% reduction in risk.15
- Decrease in red meat consumption by >0.5 servings/day was associated with a 14% reduction in risk.16
- Increase in alcohol consumption by half a glass/day among moderate drinkers was associated with an 11% reduction in risk.17
- Increase in coffee consumption by >1 cup/day was associated with an 11% reduction in risk.18
- Decrease in potato consumption by 1.0-3.4 servings/week was associated with a 6% reduction in risk.19
These recent results from studies of change within individuals in lifestyle behaviour or body weight in Swedish and US data support previous findings of associations between lifestyle behaviours measured at one time-point and incidence of type 2 diabetes. Furthermore, they provide compelling evidence that strategies aiming to shift the population distribution of risk have the potential to prevent a substantial proportion of new type 2 diabetes cases in the general population. The next step should be to develop and evaluate effective population-based strategies that could achieve a population shift in body weight and lifestyle behaviours , so that in future they can complement the existing successful high-risk strategies to reduce the burden of type 2 diabetes.
References:
- International Diabetes Federation. The Diabetes Atlas, 7th Ed.; 2015. doi:10.1289/image.ehp.v119.i03.
- Jansson SP, Fall K, Brus O, et al. Prevalence and incidence of diabetes mellitus: a nationwide population-based pharmaco-epidemiological study in Sweden. Diabet Med. 2015;32(10):1319-1328. doi:10.1111/dme.12716.
- Read SH, Kerssens JJ, McAllister DA, et al. Trends in type 2 diabetes incidence and mortality in Scotland between 2004 and 2013. Diabetologia. 2016;59(10):2106-2113. doi:10.1007/s00125-016-4054-9.
- Rose G. Sick individuals and sick populations. Int J Epidemiol. 1985;14(1):32-38. http://www.ncbi.nlm.nih.gov/pubmed/3872850.
- Gillies CL, Abrams KR, Lambert PC, et al. Pharmacological and lifestyle interventions to prevent or delay type 2 diabetes in people with impaired glucose tolerance: systematic review and meta-analysis. BMJ. 2007;334(7588):299. doi:10.1136/bmj.39063.689375.55.
- InterAct Consortium Dietary fibre and incidence of type 2 diabetes in eight European countries: the EPIC-InterAct Study and a meta-analysis of prospective studies. Diabetologia. 2015;58(7):1394-1408. doi:10.1007/s00125-015-3585-9.
- Koppes LL, Dekker JM, Hendriks HF, Bouter LM, Heine RJ. Moderate alcohol consumption lowers the risk of type 2 diabetes: a meta-analysis of prospective observational studies. Diabetes Care. 2005;28(3):719-725. doi:
- InterAct Consortium, Ekelund U, Palla L, et al. Physical activity reduces the risk of incident type 2 diabetes in general and in abdominally lean and obese men and women: the EPIC-InterAct Study. Diabetologia. 2012;55(7):1944-1952. doi:10.1007/s00125-012-2532-2.
- Abdullah A, Peeters A, de Courten M, Stoelwinder J. The magnitude of association between overweight and obesity and the risk of diabetes: a meta-analysis of prospective cohort studies. Diabetes Res Clin Pr. 2010;89(3):309-319. doi:10.1016/j.diabres.2010.04.012.
- Willi C, Bodenmann P, Ghali WA, Faris PD, Cornuz J. Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. JAMA. 2007;298(22):2654-2664. doi:10.1001/jama.298.22.2654.
- Norberg M, Wall S, Boman K, Weinehall L. The Västerbotten Intervention Programme: background, design and implications. Glob Heal Action. 2010;3. doi:10.3402/gha.v3i0.4643.
- Feldman AL, Long GH, Johansson I, et al. Change in lifestyle behaviors and diabetes risk: evidence from a population-based cohort study with 10 year follow-up. Int J Behav Nutr Phys Act. 2017;14(1):39. doi:10.1186/s12966-017-0489-8.
- Feldman AL, Griffin SJ, Ahern AL, et al. Impact of Weight Maintenance and Loss on Diabetes Risk and Burden: A Population-based Study in 33,184 Participants. BMC Public Health. 2017:17;170. doi:10.1186/s12889-017-4081-6.
- de Mutsert R, Sun Q, Willett WC, Hu FB, van Dam RM. Overweight in early adulthood, adult weight change, and risk of type 2 diabetes, cardiovascular diseases, and certain cancers in men: a cohort study. Am J Epidemiol. 2014;179(11):1353-1365. doi:10.1093/aje/kwu052.
- Ley SH, Pan A, Li Y, et al. Changes in Overall Diet Quality and Subsequent Type 2 Diabetes Risk: Three U.S. Prospective Cohorts. Diabetes Care. 2016. doi:10.2337/dc16-0574.
- Pan A, Sun Q, Bernstein AM, Manson JE, Willett WC, Hu FB. Changes in red meat consumption and subsequent risk of type 2 diabetes mellitus: three cohorts of US men and women. JAMA Intern Med. 2013;173(14):1328-1335. doi:10.1001/jamainternmed.2013.6633.
- Joosten MM, Chiuve SE, Mukamal KJ, Hu FB, Hendriks HF, Rimm EB. Changes in alcohol consumption and subsequent risk of type 2 diabetes in men. Diabetes. 2011;60(1):74-79. doi:10.2337/db10-1052.
- Bhupathiraju SN, Pan A, Manson JE, Willett WC, van Dam RM, Hu FB. Changes in coffee intake and subsequent risk of type 2 diabetes: three large cohorts of US men and women. Diabetologia. 2014;57(7):1346-1354. doi:10.1007/s00125-014-3235-7.
- Muraki I, Rimm EB, Willett WC, Manson JE, Hu FB, Sun Q. Potato consumption and risk of type 2 diabetes: Results from three prospective cohort studies. Diabetes Care. 2016;39(3):376-384. doi:10.2337/dc15-0547.

 MRC Epidemiology Unit
MRC Epidemiology Unit